Resources
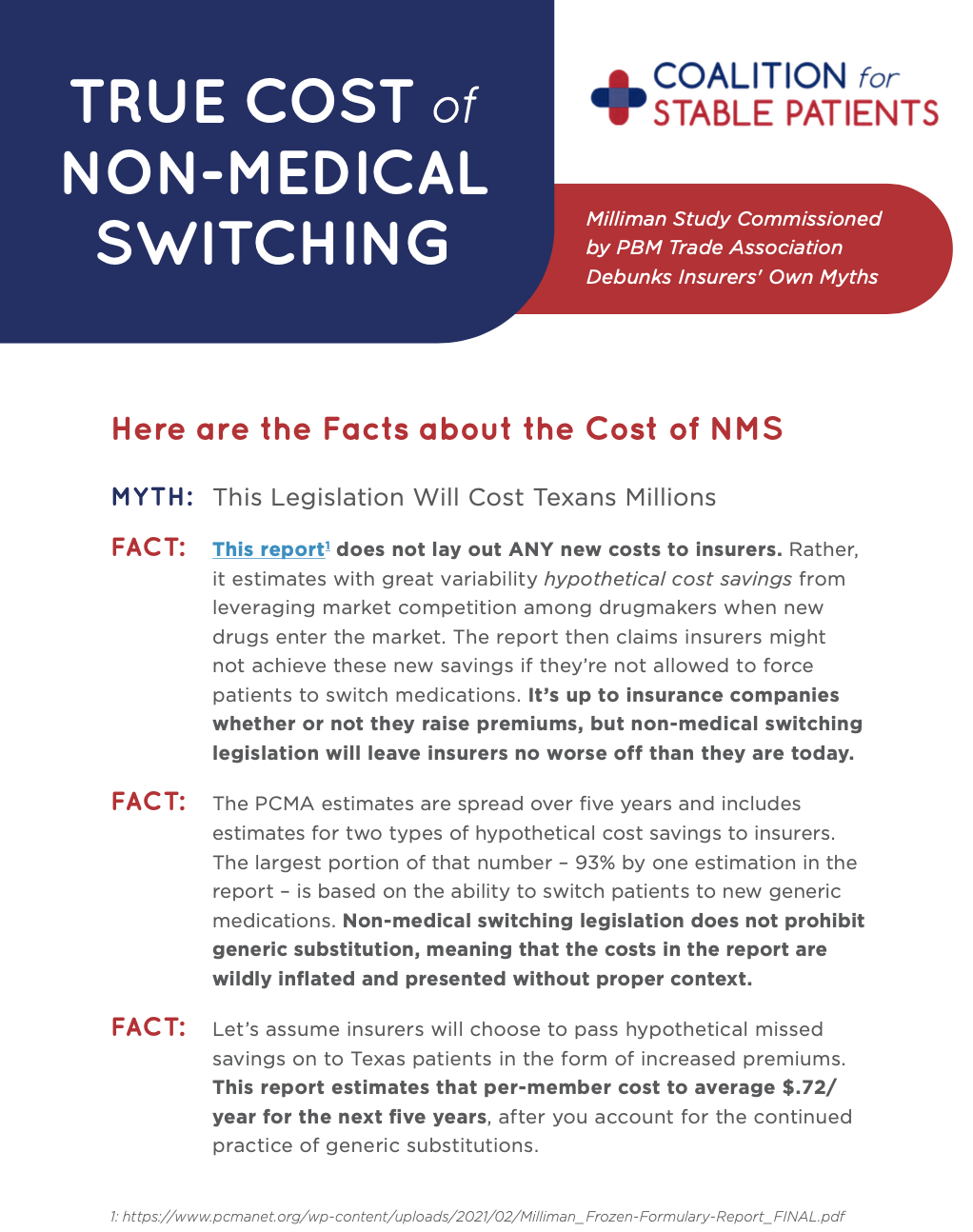
Milliman Study Commissioned by PBM Trade Association Debunks Insurers' Own Myths
MYTH: This Legislation Will Cost Texans Millions
FACT: This report does not lay out ANY new costs to insurers.
For patients living with chronic and complex diseases, it can take months or even years to find a treatment that works. But increasingly, arbitrary insurance policy changes – such as higher copays, formulary changes, or new prior authorization requirements – are forcing patients to forgo the treatments that keep them stable. That practice is called non-medical switching.
Learn more.
Myth: Health plans will have to freeze their formularies.
Fact: Health plans can continue to update their formularies as needed. They just can’t reduce coverage for patients’ preexisting prescriptions.
HB 1646 by Rep. Stan Lambert and SB 1142 by Sen. Judith Zaffirini will help Texans stay stable on medications that keep them stable, as long as they stay on the same health plan.
SB 580 and HB 2099 would end non-medical switching for people in Texas with chronic conditions. View the fact sheet to learn about the legislation and how lawmakers can ensure Texans have continued access to their prescription medications.
AfPA’s report details the findings of two in-person focus groups as well as a national poll of 800 patients who experienced non-medical switching firsthand.
Although formularies and other utilization management techniques may help contain costs for third-party payers, potential savings often come at the expense of patients’ health.
There are many myths about non-medical switching and the impact of legislation that ensures continued patient access to the treatments they need.
Patients with chronic or serious medical conditions must sometimes work with physicians for months to identify a medication that’s effective for them.
An infographic of findings from a national survey of stabilized autoimmune patients that explored their perspectives on switching prescribed biological medicines.